YOUR PHYSIO
Condition directory
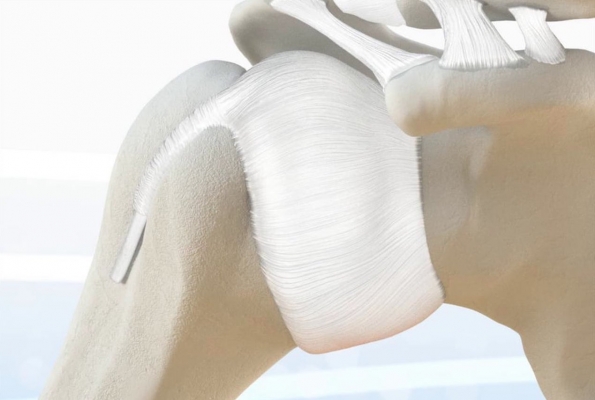
Frozen shoulder
What is Frozen shoulder?
Frozen shoulder is a condition that affects the lining of the shoulder joint. The lining becomes very inflamed (causing pain) and thickens (causing stiffness). Eventually both the inflammation and thickening lessen but this can take a long period of time, 18 months to 2 years is the average. While most people make a full recovery, about 1/3 will have some long term symptoms.
In the early stages frozen shoulders are usually characterised by severe pain , which can be worse at night and there is usually concurrent joint stiffness.
Frozen shoulders have classically been described as following a set pattern of three stages:
1. Freezing stage: the shoulder is very painful and begins to lose movement
2. Frozen stage: the shoulder is very stiff and painful
3. Thawing stage: the shoulder pain resolves and the movement slowly returns
We now know that not every frozen shoulder will follow this linear path and that the length of time for each stage will vary considerably from person to person.
A frozen shoulder can last for as little as 9 months in less severe cases, or up to 3 or 4 years in the most severe cases.
Given the often severe nature of the pain it is usually recommended that you have some treatment to improve things.
In the first instance you should speak to your First Contact Practitioner, Pharmacist, or GP about anti-inflammatory medications.
What is happening to cause the symptoms?
There is still a great deal of uncertainty as to what causes frozen shoulder. There is evidence that the bodies immune system targets the lining of the shoulder joint and that this triggers lots of inflammation (which causes the pain). As part of this process cells in the joint lining become very active and cause the lining to thicken and stick, this causes the stiffness.
Because it usually affects people at a certain age (45-65), and can run in families there is a thought that there may be a genetic link to the condition but this has not been proven.
If you are diabetic or have thyroid problems you are at a slightly higher risk of developing the symptoms, and slightly higher risk that these will take longer to go.
If your frozen shoulder has come on after a traumatic injury you should ask for a referral to us from your GP so we can make sure you haven't injured the bones or tendons.
What is the treatment?
For some people the condition will be mild and clear up on its on so no specific treatment is indicated.
For most people the pain is quite severe. As suggested above the first course of action is to get some good pain relief from your First Contact Practitioner, GP, or Pharmacist.
If these aren't working then a steroid injection into your shoulder is likely to help. Please refer yourself to the MSK team for this here.
Once your pain is under control you can then begin to gently exercise your arm. The following exercises will be helpful to maintain some movement and function in your shoulder. It is important not to over do these, as this could make your symptoms worse. As long as you are not getting lasting pain after the exercises, you can perform these as often as you like.